08/01/25
Integrative Health and Integrative Medicine: What They Are and What They Are Not
By Livy-Elcon Emereonye
In recent decades, there has been a global shift from disease-centered care toward approaches that emphasize wellness, prevention, and whole-person healing. This transformation has brought terms like integrative health and integrative medicine into mainstream conversation. While often used interchangeably, they are not the same. Both share the philosophy of treating the person as a whole rather than focusing solely on disease, but their scope, application, and practice differ. Understanding what they truly mean — and what they do not — is essential for practitioners, educators, and the public as the world moves toward more holistic and evidence-informed models of care.
The Evolution of Integrative Approaches
The origins of integrative care lie in humanity’s oldest healing traditions. Ancient medical systems — such as Ayurveda, Traditional Chinese Medicine, and African herbal medicine — emphasized balance, prevention, and connection between the body, mind, and environment. Modern biomedicine, on the other hand, has focused heavily on disease diagnosis and intervention, often leaving out the psychosocial and spiritual dimensions of health.
Over time, limitations of this reductionist model became evident. The rise of chronic, lifestyle-related diseases — such as hypertension, diabetes, obesity, and depression — revealed that pharmacological treatments alone are not enough. People began seeking complementary therapies like acupuncture, yoga, herbal remedies, and mindfulness-based stress reduction, often alongside conventional care.
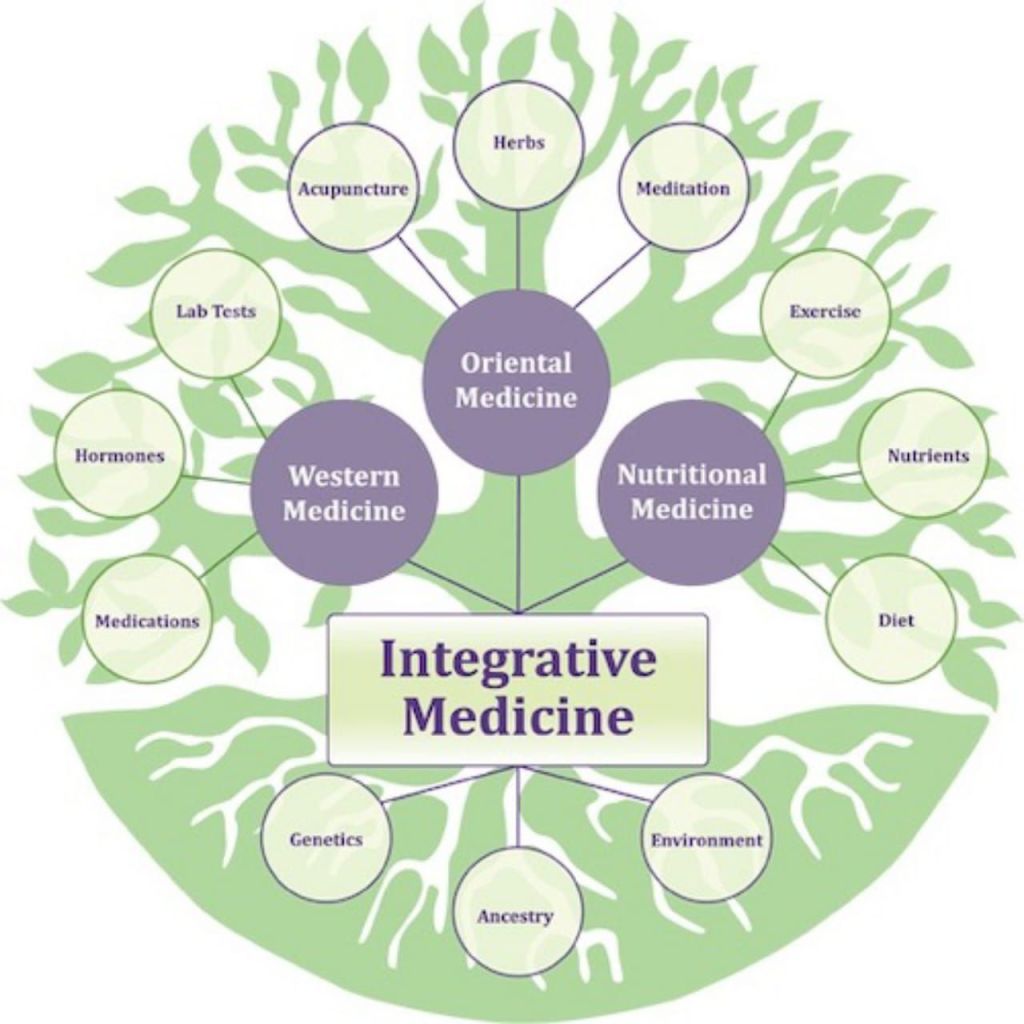
From this convergence emerged the concept of integrative medicine — a field that seeks to bring together the best of conventional and complementary practices, grounded in science, compassion, and whole-person care.
What Is Integrative Health?

Integrative health refers to the broad, holistic approach to achieving and maintaining wellbeing. It is a philosophy of health promotion that recognizes the dynamic interaction between biological, psychological, social, and spiritual factors. The goal of integrative health is not simply the absence of disease but the creation of optimal vitality, resilience, and quality of life (NCCIH, 2022).
Integrative health addresses the whole person — body, mind, and spirit — within the context of family, community, and environment. It emphasizes prevention, lifestyle change, and patient empowerment. In practice, it involves promoting nutrition, physical activity, stress management, sleep hygiene, social connection, and emotional wellbeing.
For example, an integrative health initiative may include workplace yoga programs, mindfulness training in schools, or nutrition counseling in community health centers. These programs aim to foster health literacy, prevent disease, and enhance collective wellbeing.
In other words, integrative health is a movement and philosophy focused on how to live well and stay well — a public health and community-centered approach to wellness.
What Is Integrative Medicine?
Integrative medicine, on the other hand, is a clinical practice model that combines conventional medical treatments with evidence-based complementary and traditional therapies. It is practiced by qualified health professionals — physicians, naturopathic doctors, nurses, chiropractors, herbalists, and others — who use both modern biomedical science and traditional healing systems to treat the individual holistically.
The Academic Consortium for Integrative Medicine and Health defines integrative medicine as “the practice of medicine that reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic approaches” (Consortium, 2021).
In integrative medicine, the clinician works collaboratively with the patient to create a personalized plan that might include both pharmaceutical and non-pharmaceutical interventions. For example, a patient with hypertension may receive standard antihypertensive drugs along with lifestyle coaching, stress reduction techniques, and herbal adaptogens. Similarly, a cancer patient undergoing chemotherapy might use acupuncture and mind-body therapies to relieve nausea and anxiety.
The emphasis is on safe, coordinated, and evidence-informed care, where therapies are chosen based on scientific validation and patient preference, rather than ideology.
The Common Ground Between Them
Both integrative health and integrative medicine share several foundational principles:
- Whole-person orientation: Recognizing the interconnectedness of body, mind, spirit, and environment.
- Evidence-informed practice: Integrating therapies supported by credible research, while remaining open to emerging evidence.
- Personalized care: Tailoring interventions to the individual’s unique biology, culture, and values.
- Prevention and lifestyle focus: Promoting habits that prevent disease and sustain wellbeing.
- Patient empowerment: Encouraging individuals to become active participants in their healing journey.
These shared values make integrative approaches powerful tools for both personal and societal health transformation.
How They Differ
Despite their philosophical alignment, integrative health and integrative medicine differ in scope, setting, and focus.
Aspect Integrative Health Integrative Medicine
Scope Broad, community and population level Clinical and individual level
Primary Goal Health promotion and disease prevention Diagnosis and treatment of illness
Practitioners Wellness coaches, educators, public health workers, community healers Licensed clinicians (MDs, NDs, herbalists, etc.)
Approach Lifestyle modification, education, community programs Evidence-based combination of conventional and complementary therapies
Example Workplace mindfulness and exercise initiatives Using acupuncture with chemotherapy to reduce side effects
Essentially, integrative health is the philosophy of wellbeing, while integrative medicine is the clinical expression of that philosophy.
What They Are Not
Clarifying what integrative health and integrative medicine are not is equally important.
- They are not alternative medicine.
Integrative care does not reject conventional medicine; it complements it. The aim is to use the best available evidence from all healing traditions to benefit the patient. - They are not unscientific.
Although they draw from traditional practices, integrative approaches rely on evidence-based validation. For instance, mindfulness-based stress reduction (MBSR) has strong empirical support for anxiety and chronic pain management (Kabat-Zinn, 2013). - They are not symptom-focused.
Integrative care seeks to address the root causes of illness — lifestyle, stress, environment, and emotional imbalance — rather than simply masking symptoms. - They are not a quick fix.
True healing is a process. Integrative care emphasizes long-term behavior change, prevention, and balance. - They are not exclusive to one profession.
Integrative models are collaborative, involving doctors, nurses, herbalists, psychologists, dietitians, and spiritual counselors working together.
The Evidence Base for Integrative Practice
A growing body of research supports integrative approaches in both clinical and community settings.
The World Health Organization (WHO, 2023) advocates integrating traditional and complementary medicine into national health systems to enhance accessibility and holistic care.
Studies show that combining conventional and complementary therapies can improve outcomes in chronic pain, cancer care, cardiovascular disease, anxiety, and depression (Lake & Spiegel, 2018). For example, mind-body therapies like yoga and tai chi enhance physical function and reduce stress. Nutritional interventions and herbal medicine have demonstrated benefits in metabolic and inflammatory disorders (Ulbricht et al., 2020).
Importantly, integrative medicine places strong emphasis on patient safety. The use of herbal and natural products is carefully evaluated for interactions with pharmaceuticals, and interventions are chosen based on both scientific evidence and traditional wisdom.
Global Perspectives

Across the world, health systems are beginning to embrace integrative models.
In the United States, the National Center for Complementary and Integrative Health (NCCIH) funds research and supports academic integrative medicine programs.
In China and India, integration of Traditional Chinese Medicine and Ayurveda with biomedicine is long-established and government-supported.
In Africa, the WHO Regional Office has encouraged collaboration between biomedical and traditional practitioners to improve primary healthcare delivery.
In Europe, integrative oncology and integrative mental health services are increasingly recognized for improving quality of life and reducing healthcare costs.
These global movements highlight that integrative care is not a fringe idea — it is becoming a central pillar of sustainable, patient-centered healthcare.
Integrative Health in Public Health Practice
Integrative health principles align seamlessly with public health goals. Both emphasize prevention, education, and community empowerment. By addressing social determinants of health — such as diet, environment, social support, and mental wellbeing — integrative health offers a pathway to reduce the burden of non-communicable diseases (NCDs).
For instance, lifestyle medicine, a branch overlapping with integrative health, focuses on modifying behavior through nutrition, exercise, sleep, and stress reduction. Community-based yoga and mindfulness programs have been shown to enhance mental health and social cohesion (Creswell et al., 2019).
Integrative health also supports health equity, ensuring culturally sensitive care that respects indigenous knowledge and diverse healing traditions.
Challenges and Misconceptions
Despite growing acceptance, integrative health and medicine face challenges.
Some skeptics view them as “soft science” or equate them with unregulated alternative practices. However, credible institutions are increasingly producing rigorous evidence demonstrating their efficacy. The challenge lies in standardization, regulation, and education — ensuring practitioners are qualified and therapies are validated.
Another misconception is that integrative medicine is expensive. In reality, preventive approaches often reduce long-term healthcare costs by minimizing hospital admissions and medication dependency (Dossett et al., 2020).
A final challenge is communication between practitioners. True integration requires open collaboration and respect between biomedical and traditional healers — something still evolving in many systems.
The Future of Healing
The future of healthcare is integrative.
As science continues to explore the connections between the body, mind, and environment, integrative health and medicine provide a bridge between tradition and innovation. They remind us that healing is not only about curing disease but about nurturing balance, meaning, and resilience.
Integrative care does not belong to one culture or profession — it belongs to humanity. It is the meeting point of modern science and ancient wisdom, where compassion, evidence, and experience converge for the benefit of all.
Dr. Emereonye could be reached on: +234 803 3922 445
References
Academic Consortium for Integrative Medicine and Health. (2021). About Integrative Medicine. Retrieved from https://imconsortium.org/
Creswell, J. D., Lindsay, E. K., Villalba, D. K., & Chin, B. (2019). Mindfulness training and physical health: Mechanisms and outcomes. Psychosomatic Medicine, 81(3), 224–232. https://doi.org/10.1097/PSY.0000000000000676
Dossett, M. L., Cohen, G. L., Fricchione, G. L., & Benson, H. (2020). Integrative medicine for prevention and wellness. Primary Care: Clinics in Office Practice, 47(3), 447–465. https://doi.org/10.1016/j.pop.2020.05.009
Kabat-Zinn, J. (2013). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Bantam.
Lake, J., & Spiegel, D. (2018). Complementary and alternative treatments in mental health care. American Psychiatric Publishing.
National Center for Complementary and Integrative Health (NCCIH). (2022). What is integrative health? Retrieved from https://nccih.nih.gov/
Ulbricht, C., Chao, W., & Niesen, L. (2020). Evidence-based review of herbal medicines and dietary supplements in cardiovascular disease. Journal of the American College of Cardiology, 75(10), 1239–1254. https://doi.org/10.1016/j.jacc.2020.01.037
World Health Organization (WHO). (2023). WHO global report on traditional and complementary medicine 2023. Geneva: WHO.
